“I am a doctor and a glaucoma patient. Using the iCare HOME tonometer to check my eye pressure outside of my quarterly doctor visits, gives me peace of mind.”


It is estimated that 80 million people globally are living with glaucoma
What is glaucoma?
Glaucoma is a chronic, progressive disease of the optic nerve which can eventually lead to severe visual impairment and even blindness.
Glaucoma is often completely asymptomatic in its initial stages — as glaucoma progresses, the individual may start to realize that it is getting difficult to see clearly in one or both eyes. Due to the initial lack of symptoms, it’s estimated that only 50% of glaucoma sufferers are aware that they have the disease.

Who is at risk of glaucoma?
The cause of glaucoma is still unknown, but several risk factors have been identified. Elevated intraocular pressure is one underlying risk factor for glaucoma that can be treated.

Age is a big factor too — glaucoma is rarely diagnosed in people younger than 40. The incidence of glaucoma increases with age with 2% of people over the age of 50, and 5% of people over the age of 75 living with the condition. Having close family members diagnosed with glaucoma increases the risk of having the disease three-to-nine fold. Other risk factors include severe myopia (nearsightedness) or severe hyperopia (farsightedness), and thin corneas.
Understanding your intraocular pressure
Elevated eye pressure is the only modifiable risk factor for glaucoma. An intraocular pressure between 10 and 21 mmHg is considered normal. If the intraocular pressure is in the range of 22–29 mmHg, the risk of glaucoma is ten-fold, compared to the risk for eyes with pressure in the normal range. If the intraocular pressure rises into the range of 30–35 mmHg, the risk of glaucoma increases 40-fold.
Elevated intraocular pressure is likely to cause glaucoma in two ways. Firstly, by direct pressure exerted on the fibers of the optic nerve. Secondly, by adversely affecting the blood flow in the head of the optic nerve and its metabolism.
If you have had a high reading from an intraocular pressure measurement, it is advisable to consult an ophthalmologist.
In addition to elevated intraocular pressure, variation in intraocular pressure may also be associated with glaucoma. In healthy eyes, the variation in intraocular pressure is low, but in glaucoma, it may be significant. Peaks in intraocular pressure can occur at any time of the day or night.

Why are frequent IOP measurements crucial to glaucoma care?
Currently, lowering intraocular pressure is the only treatment for glaucoma. The primary objective of glaucoma therapy is to prevent glaucoma-induced visual impairment. Treatment of the disease is based on reducing IOP, regardless of the base level. The normal goal is to lower IOP by 20–30% or at least lower it to a level below 20 mmHg.

The most common treatment for glaucoma is the use of eye drop medication. The effectiveness of the medication is assessed by monitoring the reduction in eye pressure, imaging the optic nerve head and nerve fibers, as well as testing the visual field. If medication is not suitable or is ineffective, laser or surgical treatment may be considered.
Regular measurement of intraocular pressure is an important factor for the early detection of glaucoma. The prognosis for glaucoma is generally good if the disease is detected early and the patient adheres to treatment and follow-up. The greatest risk of visual impairment comes with delayed detection of glaucoma.

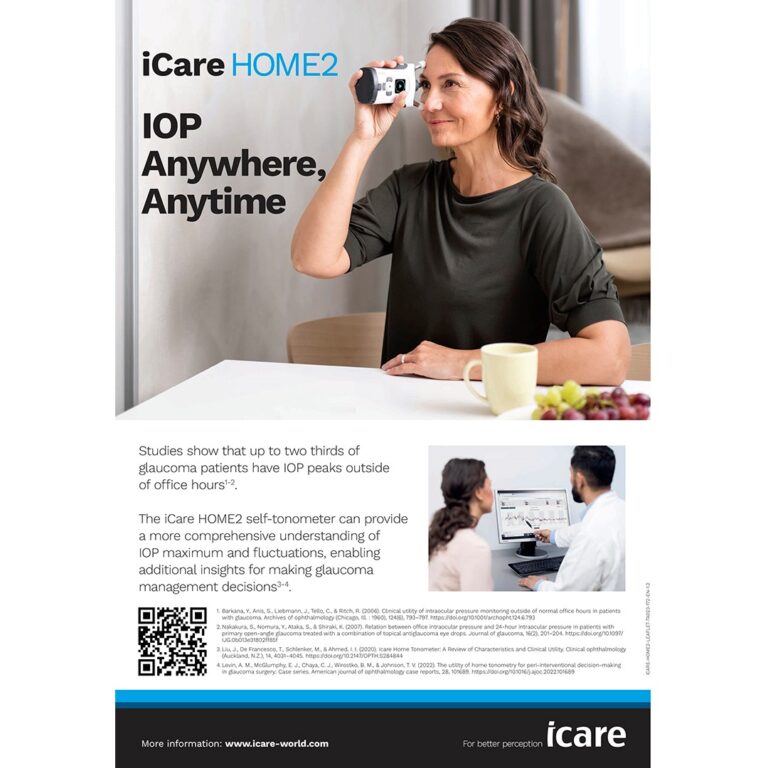
Intraocular pressure can vary throughout the day and night and on different days, especially in glaucomatous eyes. Therefore, there is a high probability of missing important IOP peaks if only sporadic IOP measurements are taken during office hours. With the iCare HOME2, you can be sure that your doctor has access to all the important information to help them make timely decisions based on ample, real-world data.
The information on this site is sourced from: glaucomapatients.org, and glaucoma.org published by the Glaucoma Research Foundation and the World Glaucoma Association.

iCare HOME2
• Advanced tonometry technology for accurate results
• Ergonomic design with adjustable forehead and cheek support
• Device that requires no calibration and minimum maintenance
• Smart light guide and screen that assists you with measurements
• Accurate measurement error detection
• Compact, lightweight, and travel-friendly device with a custom-designed case
Print the iCare HOME2 leaflet with you to give to your doctor
Download the leafletFAQ
-
What do the eye pressure values mean for me? When should I be concerned about the eye pressure readings?
Intraocular pressure (IOP) is the fluid pressure in the eye and is also known as eye pressure. IOP is only one aspect of eye health and glaucoma. IOP values alone cannot be used to diagnose accurately or monitor glaucoma.. Saying this, IOP reduction is still the only proven method for slowing glaucomatous progression.
Having an accurate overview of your diurnal IOP profile may assist your eye care professional in tailoring a management program to suit your individual needs. You should always discuss any IOP concerns with your eye care professional, to ascertain what normal looks like for you. Every glaucoma patient is different.
-
How do I show my results to my eye care professional (ECP)?
You can show your results in several ways:
- Directly on the iCare PATIENT2 app on your phone
- Print out or email a report from the computer
- You can ask your ophthalmologist to subscribe for the iCare CLINIC software so that they can view your measurement results online
-
Does it hurt?
Measurement is painless. The light-weight probe touches the cornea momentarily and some patients don’t even notice the measurement.
-
How often should I calibrate the tonometer?
The tonometer does not require any routine servicing or calibration. If there is a reason to believe that the servicing of the tonometer is necessary, contact the local distributor or the manufacturer.
-
How often should I change the probe?
The probes are for single use (single pair of measurement sequences) only. Each probe can be used once to take a successful measurement in both eyes. If you eye is inflamed or infected, measure the healthy eye first.
-
How often should I change the probe base?
Every 6 months is recommended to maintain the accuracy of the device.
-
Where can I find all the iCare self-tonometer instruction manuals and materials?
You can find all the manuals and materials on the iCare USB drive, located inside the iCare carrying case. You can also download digital versions from our website.
-
How do I clean my tonometer?
You can clean the plastic surfaces with a cloth or a paper towel dampened with water.
-
Can I travel with the tonometer?
Yes, you can take the tonometer anywhere with you.
Patient testimonials
-
-
”The iCare HOME saved my sight. After taking my eye pressure at home, the
doctor changed my treatment plan, which slowed my glaucoma progression.” -
”I started using the iCare HOME just in time to save vision in my right eye, I wish I had access sooner for my left eye.”
Related articles
-
Where to buy?
Local qualified iCare retailers are ready to help you with all matters related to iCare products and services. Click to see your local retailer.
More information -
Subscribe to our newsletter
Click here


